by Emma Nelson
Pain is a very difficult concept to grasp with many unknowns but within the past 10 years, there has been more research that has provided more information. As health care professionals, we are constantly trying to find the root cause of pain to try to alleviate it. There are many sources of pain which is why it is a difficult problem to solve but with more education on the topic, that has been shown to decrease pain levels in some people. By providing some information about pain science, I hope to increase your knowledge on pain to better understand the process you may be experiencing.
According to the International Association for the Study of Pain, their current definition is “An unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage.” This definition has evolved to include potential tissue damage meaning that there could be no physical damage structurally, but you can still experience pain from a variety of other causes.
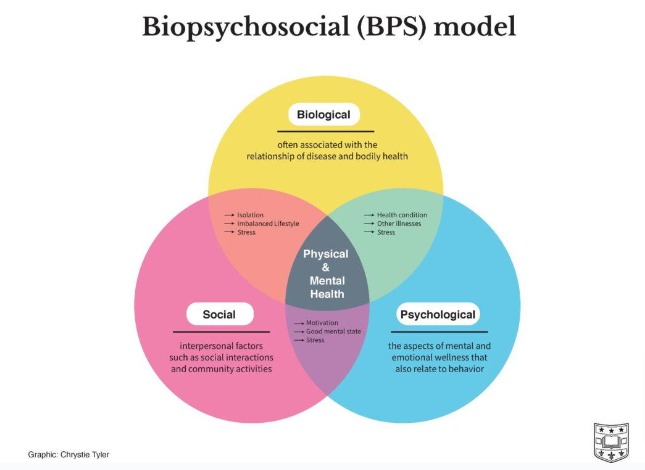
The biopsychosocial model is used to break down potential factors that could be contributing to your pain. There is a biological, psychological, and social component of this model. Please see the diagram below which describes potential contributors to your pain.
Have you ever wondered why sometimes your pain feels like a sharp shooting sensation and sometimes it is a dull-achy feeling? Or even why some pain lasts for short periods of time and other pain sensations last longer? That is because there are various types of pain, and each can present differently. Pain can be classified by how long it lasts such as acute (shorter periods of time) or chronic pain (longer lasting). Pain can also be classified by the mechanism of the pain which can include nociceptive, nociplastic, and neuropathic pain.
Nociceptive
- Pain is perceived because the sensory receptors in various locations in your body are detecting a painful stimulus which could be inflammation, a mechanical irritant, or due to an injury.
- Examples: Knee osteoarthritis or ankle sprain
Nociplastic
- This pain is typically longer lasting because it is not just involving sensory receptors located around your body, there is something that is disrupting the processing in your brain. Nociceptive pain can turn into nociplastic pain. There could have been an initial injury, and the physical part has healed, but there you can still experience pain due to your processing centers in your brain being altered.
- Examples: Fibromyalgia and non-specific low back pain
Neuropathic
- This is pain that is caused by a lesion or disease to the nervous system (brain, spinal cord, or nerves).
- Examples: Carpal tunnel syndrome and diabetic neuropathy
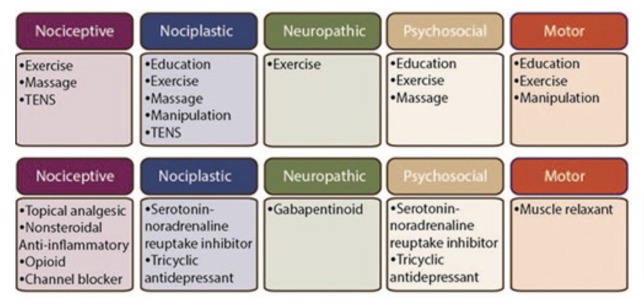
There are specific treatments for the type of pain that you have. You will have to discuss your symptoms with a medical professional to see the best treatment options. The figure below shows potential treatments that may be considered for each type of pain.
The most important thing to take away from the figure above is that exercise has been shown to improve pain levels for all types of pain. It is critical to incorporate exercise into your daily routines to help decrease pain levels. If you are experiencing pain and it is impacting your daily function, it is important to reach out to a physical therapist. Physical therapists can provide more information on potential reasons why you are experiencing your pain, deliver treatments to target your specific pain, and help you incorporate exercise into your life. We can also refer you to medical professionals to best manage your pain levels. Overall, pain is experienced by many individuals and by knowing why you are experiencing your pain may help to start alleviating it. I hope that this information provided above expanded your knowledge on pain science and increases your awareness of potential ways physical therapists and other health care professionals can help manage your pain.
References
- Chimenti RL, Frey-Law LA, Sluka KA. A Mechanism-Based Approach to Physical Therapist Management of Pain. Phys Ther. 2018;98(5):302-314. doi:10.1093/ptj/pzy030
- Darnall BD, Roy A, Chen AL, et al. Comparison of a Single-Session Pain Management Skills Intervention With a Single-Session Health Education Intervention and 8 Sessions of Cognitive Behavioral Therapy in Adults With Chronic Low Back Pain: A Randomized Clinical Trial. JAMA Netw Open. 2021;4(8):e2113401. doi:10.1001/jamanetworkopen.2021.13401
- Pain Neuroscience Education (PNE). Physiopedia. Accessed February 8, 2024. https://www.physio-pedia.com/Pain_Neuroscience_Education_(PNE)
- Louw A, Puentedura EJ, Diener I, Zimney KJ, Cox T. Pain neuroscience education: Which pain neuroscience education metaphor worked best? S Afr J Physiother. 2019;75(1):1329. doi:10.4102/sajp.v75i1.1329
- Physical Activity for Pain Prevention. International Association for the Study of Pain (IASP). Accessed February 8, 2024. https://www.iasp-pain.org/resources/fact-sheets/physical-activity-for-pain-prevention/
- Raja SN, Carr DB, Cohen M, et al. The Revised IASP definition of pain: concepts, challenges, and compromises. Pain. 2020;161(9):1976-1982. doi:10.1097/j.pain.0000000000001939
- Three Aspects of Health and Healing: The Biopsychosocial Model in Medicine | Department of Surgery | Washington University in St. Louis. Accessed February 8, 2024. https://surgery.wustl.edu/three-aspects-of-health-and-healing-the-biopsychosocial-model/